Exciting new and ongoing developments in chimeric antigen receptor (CAR) T-cell therapies were covered at the 62nd American Society of Hematology (ASH) annual meeting.
Exciting new and ongoing developments in chimeric antigen receptor (CAR) T-cell therapies were covered at the 62nd American Society of Hematology (ASH) annual meeting.

An investigational drug, IMM-101, already being studied for its ability to increase the effects of immuno-oncology agents, may be able to prevent or lessen the effects of COVID-19 among those with cancer.
Evidence-Based Oncology managed care updates for August 2020 feature coverage of liquid biopsies, companion diagnostics, and CAR T-cell therapy.

The oncology drug pipeline has experienced rapid growth over the past decade, driven by innovation in cell therapies, immunotherapy, and precision medicine, according to a specialty pipeline update presentation at Asembia's 15th annual Specialty Pharmacy Summit, held April 29 to May 2 in Las Vegas.

The breast cancer community is very excited about the approval of atezolimuab for the treatment of triple-negative breast cancer, explained Lee Schwartzberg, MD, FACP, executive director, West Cancer Center.

Administration of immuno-oncology therapy for cancer diagnoses in the community clinic setting is associated with lower costs compared with administration in a hospital-based clinic setting.

This week, the top managed care news included increased demand for long-acting contraception since President Trump took office; a payer decision on an insulin pump alarmed diabetes advocates; and despite being involved in cancer treatment decisions, many primary care providers don't feel prepared to do so.

Evidence-Based OncologyTM recently sat down with Rodabe Amaria, MD, assistant professor in the Department of Melanoma Medical Oncology, Division of Cancer Medicine, at MD Anderson and a lead author on a study that found that evidence has been accumulating in preclinical models that neoadjuvant treatment may be superior to treatment after surgery for patients with advanced melanoma.

Immunotherapy has seen great success in the treatment of numerous cancers, from melanoma to lung, breast, colorectal, kidney, and even some brain cancers. But thus far, despite several attempts, the devastating brain disease glioblastoma has not been among the immunotherapy success stories. In fact, glioblastoma researchers have had few advances in more than a decade.
Higher tumor mutational burden is associated with improved overall survival in patients with stage IV or metastatic disease being treated with immune checkpoint inhibitors.
As new, innovative therapies with high price tags, such as chimeric antigen receptor (CAR) T-cell therapy, come to market, the US health system will have to start looking at different approaches for reimbursement, said Ted Okon, MBA, executive director of the Community Oncology Alliance.
A recent trial looked to compare the efficacy and safety of pembrolizumab (Keytruda) with the standard of care for the treatment of head and neck squamous cell carcinoma (SCC).

Earlier this week, the FDA granted accelerated approval to pembrolizumab (Keytruda) for adult and pediatric patients with recurrent locally advanced or metastatic Merkel cell carcinoma (MCC).

Patients with advanced cutaneous melanoma who are responsive to nivolumab (Opdivo) have higher serum levels of soluble CD163 (sCD163) compared with nonresponders, according to the results of a recent study.

The Allen Institute for Immunology has partnered with several cancer institutions, including the Fred Hutchinson Cancer Research Center, with the primary goal of understanding the differences between a defective and healthy immune system to improve immune-based treatments.

While patient-reported outcomes don’t provide the whole story, they can provide insight into how chimeric antigen receptor (CAR) T-cell therapy changes a patient’s life, said Brian Koffman, MDCM, DCFP, DABFM, MS Ed, medical director, CLL Society.
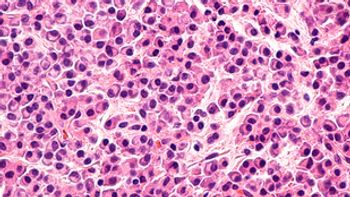
A median 19-month follow-up of the JULIET trial—a single-arm, open-label, multicenter, global, pivotal phase 2 trial of the chimeric antigen receptor-T cell therapy tisagenlecleucel directed against CD19-expressing B cells—has found a 40% complete response and a manageable safety profile in adult patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL).
Researchers at the 60th American Society of Hematology Annual Meeting & Exposition presented long-term study results showing that high rates of minimal residual disease–negative complete response were sustained with a median duration of over 4 years among treatment-naïve patients with multiple myeloma.

This study assesses the value of novel immuno-oncology treatments to society.

While new therapies like chimeric antigen receptor (CAR) T-cell therapy, can have amazing results, the innovation of these treatments has outstripped the United States’ ability to pay for them, said Michael Kolodziej, MD, vice president and chief innovation officer at ADVI Health, Inc.

A multicenter retrospective study that evaluated the efficacy and safety of chimeric antigen receptor (CAR) T-cell treatment, axicabtagene ciloleucel (axi-cel; Yescarta), in a real-world setting found a similar response as well as toxicity compared with the ZUMA-1 clinical trial.
This week, the FDA approved larotrectinib, to be sold as Vitrakvi, for the treatment of adult and pediatric patients with solid tumors that have a neurotrophic receptor tyrosine kinase (NTRK) gene infusion without a known acquired resistance mutation, are metastatic or where surgical resection is likely to result in severe morbidity, and have no satisfactory alternative treatments or that have progressed following treatment.
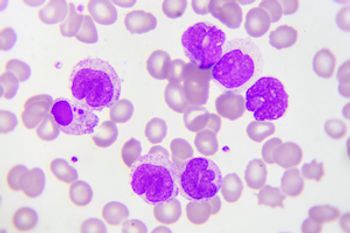
CD7 gene-edited chimeric antigen receptor (CAR) T cells target CD7-positive acute myeloid leukemia (AML) cells while sparing myeloid and erythroid cells and minimizing toxicity, according to the results of a recent study.

After being treated for his chronic lymphocytic leukemia with chimeric antigen receptor (CAR) T-cell therapy, Brian Koffman, MDCM, DCFP, DABFM, MS Ed, medical director, CLL Society, is being followed for 15 years to better understand if there are any undiscovered adverse events that pop up and how durable the response is.

Earlier this month, Merck announced that the FDA approved its anti–PD-1 therapy, pembrolizumab (sold as Keytruda), for the treatment of patients with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
