Oncology
Latest News
Latest Videos

Podcasts
CME Content
More News

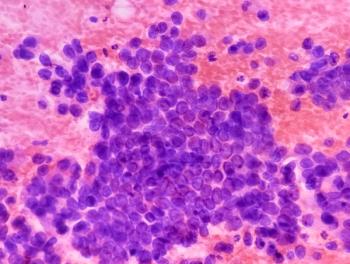
Super-enhancer-related microRNAs (miRNAs) reveal diverse subtypes of small cell lung cancer (SCLC), offering potential as diagnostic and prognostic biomarkers.

Community oncology leaders navigate challenges in value-based care under the Enhancing Oncology Model, facing performance payment uncertainties and evolving drug markets.
FDA expands selumetinib approval to younger children with NF1-related tumors.

Subcutaneous amivantamab plus chemotherapy offers an equally effective treatment for EGFR exon 20 insertion non–small cell lung cancer (NSCLC), mirroring PAPILLON results of the intravenous formulation, explained Sun Lim Min, MD, PhD.

Disparities in lung cancer biomarker testing show barriers that delay diagnosis and treatment for lower-income patients, according to Sandip P. Patel, MD.

Personalized testing is preferred for patients with NSCLC with mutations, but there are challenges to implementing this testing, said Yang Xia, MD, PhD.
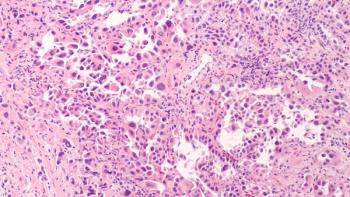
Uncommon EGFR mutations in non–small cell lung cancer (NSCLC) remain challenging to treat, but new tyrosine kinase inhibitors, bispecific antibodies, and a proposed “PACCage insert” framework provide opportunities to advance precision therapy.
Treatment of EGFR-mutated non–small cell lung cancer (NSCLC) is shifting toward next-generation sequencing and combination regimens that improve survival but increase toxicity, requiring individualized care.

Antibody-drug conjugates are rapidly reshaping the treatment landscape of non–small cell lung cancer (NSCLC), with advances in design, clinical efficacy, and regulatory approvals tempered by ongoing challenges in toxicity, resistance, and biomarker optimization.
Bispecific antibodies are emerging as a transformative class in advanced non–small cell lung cancer (NSCLC), with agents such as amivantamab and zenocutuzumab already demonstrating clinical benefit and a broad pipeline of investigational therapies showing promise in overcoming resistance.

National Comprehensive Cancer Network (NCCN), the European Society for Medical Oncology (ESMO), and the American College of Chest Physicians (CHEST) offer complementary yet distinct frameworks for lung cancer care, reflecting differences in evidence evaluation, regional adaptation, and policy integration.

Oranus Mohammadi, MD, outlines how antibody-drug conjugates are transforming breast cancer treatment across subtypes and discusses her approach to sequencing high-cost targeted therapies within payer and clinical practice constraints.

Oranus Mohammadi, MD, discusses the emerging applications of circulating tumor DNA (ctDNA) in breast cancer care and emphasizes the importance of clear communication to help patients navigate uncertain or anxiety-provoking biomarker test results.

Patients with small cell lung cancer (SCLC) experienced better responses to immune checkpoint inhibitors if they had higher levels of NOTCH1 expression in a recent study.

Joanne Mortimer, MD, FACP, FASCO, discusses the practical applications and limitations of circulating tumor DNA (ctDNA) testing in breast cancer, highlighting its role in guiding targeted therapy, challenges in patient communication and payer coverage, and unique barriers for male patients.

Jorge Nieva, MD, explores the challenges of translating biomarker testing into treatment decisions for non–small cell lung cancer (NSCLC), the role of repeat testing in detecting resistance mutations, and the importance of equitable access to molecular diagnostics in value-based care settings.
The findings may inform future studies on the therapeutic strategy for patients with small cell lung cancer (SCLC).

The 6-month progression-free survival rate for the combination therapy was 52.2%.
Jorge Nieva, MD, highlights the critical role of molecular testing in non–small cell lung cancer (NSCLC) care, while addressing barriers such as limited tissue samples, delayed turnaround times, and the need for faster, more accessible diagnostic technologies.

Yale Podnos, MD, MPH, FACS, discusses strategies to address social determinants of health in oncology, improve clinical trial enrollment for underserved communities, and leverage value-based care models to reduce financial toxicity and ensure equitable cancer care.

Daniel Virnich, MD, highlights the need for proactive social determinants of health screening, language-inclusive clinical trial practices, value-based treatment decisions, and policy reforms to improve equitable access to cancer care.

Lauren Antrim, MD, of City of Hope Cancer Center Duarte, emphasized the need for more evidence to guide optimal immunotherapy duration and sequencing in in non–small cell lung cancer (NSCLC), highlighting ongoing trials and the potential role of ctDNA in tailoring treatment strategies.

Housing assistance significantly reduces medical financial hardship for renters with a history of cancer, enhancing their financial security and access to care amid rising health costs.

Lauren Antrim, MD, emphasized the need to balance safety, efficacy, and financial considerations when managing immune checkpoint inhibitors in NSCLC, underscoring the importance of patient-centered discussions and ongoing trials to refine treatment duration strategies.

The study found no difference in physician communication scores between patients with advanced cancer and other illnesses, suggesting that discordance may stem from other dynamics.