Insurance
Latest News
Latest Videos

More News

The health care provisions include key reforms targeting pharmacy benefit managers, extensions of Medicare telehealth flexibilities, and measures aimed at combating the opioid crisis and preparing for future pandemics.

A new report from The Commonwealth Fund compares trends in health plan spending and employee costs for 2014 through 2023 between small and large businesses, taking into account plan premiums, employee contributions, and deductibles. It also highlights that although small firms do not even have to offer health benefits, large firms are required to do so by the Affordable Care Act.


This study found widespread instances of disconnect in online provider directories between information needed by patients and data availability.

Among commercial and Medicare supplemental beneficiaries with cost sharing, higher out-of-pocket spending for the first cardiac rehabilitation session was associated with lower program adherence.

Older adults in the United States are disproportionately affected by health care costs compared with their counterparts in other wealthy nations.

While the Medicare Competitive Bidding Program reduced spending, it did not significantly impact supplemental oxygen use or clinical outcomes among patients with chronic obstructive pulmonary disease (COPD).

The Wellness Way facility was designed to improve access to comprehensive outpatient care and address social determinants of health for a diverse patient population.

Despite significant progress in expanding health insurance coverage since the Affordable Care Act (ACA) was enacted, millions of Americans still face critical gaps in access to and affordability of health care.

At CAQH Connect 2024, health care leaders discussed advancing value-based care through collaboration, data standardization, patient-centered approaches, and adaptable partnerships.

This survey assesses physician experiences with utilization management and burnout and investigates whether there is a link between them.

Medicaid and CHIP enrollment surged from 71 million in February 2020 to 94 million by April 2023. However, with the pandemic emergency ending in May 2023, states resumed eligibility reviews, initiating a process termed “unwinding.”

As Cigna and Humana pick back up on the potential for a megamerger, executives will be keeping a close eye on the outcomes of the presidential election.

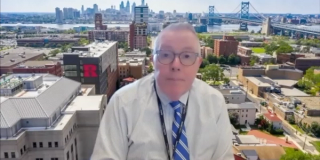
Carol R. Regueiro, MD, MSc, of Allegheny Health Network, highlights how the Physician Partners of Western PA practice support model has successfully engaged specialty practices to enhance patient connections and promote a population health perspective.

This week’s Center on Health Equity & Access highlights emphasize the role of social determinants of health in policy-making and underscore the importance of addressing rising costs and challenges employers face.

Carol R. Regueiro, MD, MSc, of Allegheny Health Network (AHN), explains how AHN's congestive heart failure bundle has enhanced collaboration between cardiology and primary care.

In the wake of the Inflation Reduction Act and other regulatory changes, Medicare Advantage plans have braced for significant cuts that are forcing them to take a hard look at their product offering.

Report reveals growing divide between subsidized and unsubsidized enrollees.

Program yields largest savings in its history of more than $2.1 billion in 2023.

The US should consider reducing or eliminating employer-sponsored insurance. Here are some ways to do it efficiently.

Carol R. Regueiro, MD, MSc, of Allegheny Health Network, described how AHN's Physician Partners of Western PA practice support model and shadow bundle distribution model enhanced collaboration between primary and specialty care to improve patient outcomes.

Cost avoidance varied by clinical setting, with the largest savings occurring in hematology clinics ($73,773), followed by rheumatology ($45,330) and pediatric gastrointestinal/irritable bowel syndrome ($16,519).

The Medicaid budget survey for fiscal years 2024 and 2025 revealed state predictions are expecting a decline in Medicaid enrollment and an increase in spending next year due to the end of pandemic-era policies and federal funding.

On this episode of Managed Care Cast, we're talking with the author of a study published in the October 2024 issue of The American Journal of Managed Care® that explored prior authorization decisions in cancer care by race and ethnicity for commercially insured patients.

Medicaid expansion is associated with improved care and increased survival rates for patients with certain breast cancers, but future studies should focus on whether Medicaid expansion mitigates the disparities between Black and non-White patients.